What Happens After a Stroke?
What is Happening in the Brain After a Stroke & Why?
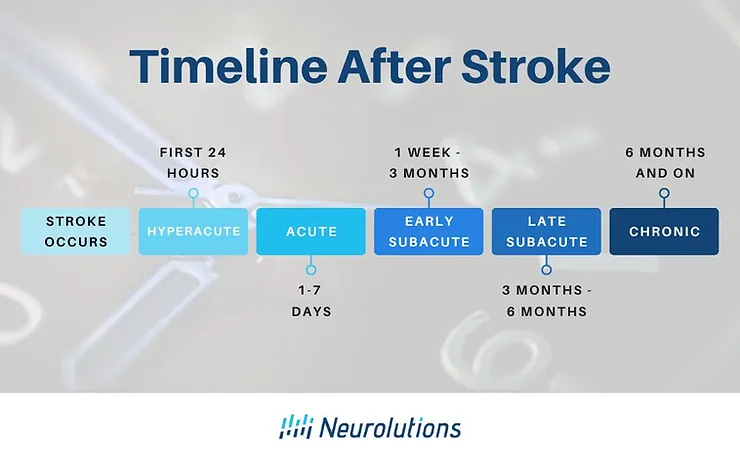
The chronological timeline commonly following the initial symptoms of a stroke is often divided into five separate phases. These phases in the post-stroke timeline are based on what is happening in the brain from a structural standpoint as the brain repairs and heal itself from a stroke.
Why does all of this neuroscience matter?
If you or your loved one has had a stroke, having this knowledge of the phases can be powerful to help you understand what is happening in the brain so you can take the right steps to get the care you need along the timeline.
This article will discuss what is happening in the brain-based timelines post-stroke, key takeaways, and most importantly an overview of how to take action to optimize recovery potential.

Phases of Stroke Organized by Timeline
The biological phases, agreed upon by The Stroke Recovery and Rehabilitation Roundtable Taskforce (1), are as follows:
Phase of Stroke Elapsed time since stroke
- Hyperacute: First 24 hours
- Acute:1-7 days early
- Subacute: 7 days – 3 months
- Late Subacute: 3 – 6 months
- Chronic: > 6 months through the remainder of the lifespan
Let’s dive into what is happening in the brain as well as key takeaways during each of these phases
Are you finding this article helpful? If you or a loved one has been impacted by stroke, the Neurolutions IpsiHand could help.
The Hyperacute Phase of Stroke: the first symptom of a stroke to 6 hours
When a stroke occurs, the brain’s blood supply in certain regions is disrupted and a core of neuronal tissue dies. There is swelling within the brain as well as a loss of oxygen and nutrients. Because strokes cause damage to the brain and the brain is a vital organ to sustain bodily functions, having a stroke is a medical emergency.
The individual needs to get to a hospital as fast as possible so the stroke team can focus on saving their life, saving the brain, and controlling other organ systems in the body from failing.
Key Takeaways: Cell death and swelling is happening because of the stroke. Every second counts to save the brain.
How to Take Action: React quickly. Follow the guidance using the acronym BE FAST (insert figure). Get to the hospital ASAP if you know something is wrong.
The Acute Phase of Stroke: the first seven days
In the acute stages post-stroke, there is an area around the dead tissue known as the penumbra. The penumbra makes up the billions of brain cells that envelop the dead tissue.
Although these cells may be failing and are temporarily non-functional, they are still viable and may return from a state of shock. This process is known as diaschisis and serves as the mechanism of what is called spontaneous recovery.
Spontaneous recovery is unrelated to the improvements that can be made by therapy. It is the rapid and significant functional improvement that can sometimes occur in the acute phase after stroke but also occurs well into the next phase of stroke- the early subacute phase.
Key Takeaways: Depending on the severity and location of the stroke, you may see rapid and significant improvement in the early days in the hospital.
Take Action: In the acute phase of stroke, treatment is focused on bedside therapy. While intensive therapy is not advised in the acute stage, you still should be participating in therapy that is considered “tolerated” and when you are most alert. Most therapy can be done within the hospital room at the “bedside.” Activities guided by therapists, nursing staff, and even family members should encourage attempts to perform basic movements (e.g. rolling, scooting, standing up and sitting down, transfers to different chairs or the commode, short walks, reaching, and opening and closing the hand.)
Compensation should be limited in the acute phase! Training focusing on the “good” side worsens future function of the “bad” side if done for the first 10 days.” (3)
The Early Subacute Phase of Stroke: 7 days to 3 months
When a patient is cleared to begin stroke rehabilitation after the acute stage is over, the key to subacute stroke recovery in the weeks that follow is to tap into “plasticity” mechanisms in the brain. The goal is to wake up areas of the brain that have not been damaged. Interventions that promote reorganization within intact brain areas and “save the penumbra” rewire brain cells together by forming new connections.
The problem with the penumbra is that it takes hard work to use the brain cells again. Stroke recovery is frustrating because there is a lot of trial and error on behalf of the survivor. It is not unusual for the stroke survivor to compensate or adapt to make a task easier or for their loved one to over-help. Unfortunately, this does not help brain cells get back online again.
Key Takeaways: The brain is good at “use it or lose it.” So, “use it to improve it!” Therapy should now become more intensive because brain plasticity is enhanced in this phase.
Take Action: The goal is to restore– not compensate! Recovery should be more intense.
Because the subacute phase is such a pivotal point in your recovery, be sure you ask for rehabilitation to help you recover. You will learn a lot from your well-trained therapists. Do not try to rehabilitate on your own. Be agreeable to trying even though it will be frustrating and you might be a little fearful. They will help you level up!
The Late Subacute Phase of Stroke: 3 to 6 months
Neurons that were “offline” may have become “online” again because of rehabilitation efforts and natural biological recovery. However, these online neurons are not quite the same. They are trying to adapt and find new pathways to reroute around damaged pathways, but they still may be sluggish. This means that you may be moving or thinking slower without the accuracy you once had.
Key Takeaways: Many individuals find themselves having highs and lows in their recovery. The psychological battle also weighs heavily on a person, because the individual is trying to get back on track with their life and they feel held back. Therapy can be exhausting just as it can be exhilarating.
Take Action:
Keep fighting the good fight. Realize this is often a marathon and not a sprint. A little progress every day can lead to big achievements.
Although this may not be your typical personality, adopt a stubborn, “let me do this!” mentality. When you force your own brain to think and try- much like when you were learning as a child- you will be better off in the long run.
The Chronic Phase of Stroke: 6 months and through the rest of the survivor’s life
From a cellular standpoint, neural repair before entering the chronic phase has already taken place and conditions are relatively “stable.” Surviving neurons are either working efficiently, sluggish or everything in between. When neurons are sluggish and become lazy, the connections they have between other neurons become “pruned,” or cut off. This means that big improvements and the chances for spontaneous recovery is not as likely. Individuals avoid, forget, or become more resistant to start using their affected side, which becomes a detrimental process known as learned non-use.
There is hope, however!
Those in the chronic phase post-stroke have more recovery options than ever before. Additionally, emerging research is concluding that the brain can make positive changes toward functional improvement under the right conditions that promote neuroplasticity. For more information, refer to our Complete Guide to Chronic Strokes.
Key Takeaways: While progress does often slow in the chronic phase after stroke, it is still possible. Don’t accept plateaus. There is always a way to keep pushing to break through the walls.
Take Action: Continue with rehabilitation you consider challenging and intensive, if possible.
Keep progressing with the exercises/activities that have become too easy for you. It is also good to switch up your routine to challenge the brain and body with new activities.
You may have to do therapy from home on your own without regular rehabilitation. It is still possible to be successful through home rehabilitation. Have your therapist design a challenging yet safe plan for you, incorporating a method to record your progress along the way to stay motivated and be accountable for hitting certain milestones.
Be open to trying new technologies so long as you have received education on the purpose and the goal.
How Long Does It Take To Recover From a Stroke?
Post-stroke rehabilitation is key to recovery. Although understanding these timelines can be helpful, interpretation of the timeline should always be taken when it comes to applying it to YOUR recovery.
Why?
Every person is different. Every stroke is different. Rehabilitation experiences are even different!
You are not locked in as much as you have been told.
The greatest enemy to stroke recovery is setting limits on how far you can go.
Brain recovery is not entirely a passive process.
It relies on YOU- your persistence in rehabilitation, your support system, and expanding the resources you have around you- to get to where you want to go.
This should be good news once you realize you can be a warrior and come out on the other side victorious.
For more information about the long-term symptoms, stroke survivors may experience, refer to our Complete Guide to Chronic Strokes
References:
————————-
(1) Bernhardt, J., Hayward, K. S., Kwakkel, G., Ward, N. S., Wolf, S. L., Borschmann, K., et al. (2017). Agreed definitions and a shared vision for new standards in stroke recovery research: The stroke recovery and rehabilitation roundtable taskforce. Neurorehabilitation and Neural Repair, 31, 793–799.
(2) Jones TA. Motor compensation and its effects on neural reorganization after stroke. Nat Rev Neurosci. 2017;18(5):267-280. doi:10.1038/nrn.2017.26