Cervical spondylosis (CS) and heart palpitations are conditions individuals are more likely to encounter as they age. CS is a painful degenerative condition of the neck vertebrae and most often caused by arthritis. According to the American Academy of Orthopaedic Surgeons, 85% of all adults above age 60 have CS (1). Separately, heart palpitations are common in adults for a variety of reasons, with chronic stress being a major cause that can lead to heart rhythm disorders.
The following article describes CS and heart palpitations (including their diagnosis and management), as well as their link to increased stroke risk.
What is Cervical Spondylosis?
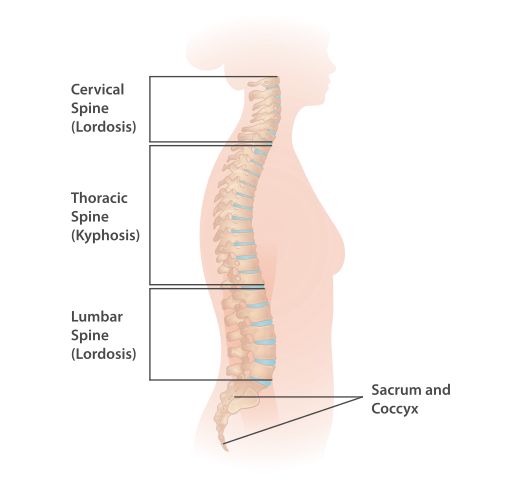
The spine is composed of 33 small bones called vertebrae (2). These bones are connected to each other by soft tissue called cartilage. Cartilage cushions the bones of the spinal column from rubbing against each other. Cartilage loss can cause both pain and pressure on spinal nerves. The vertebrae that form the spinal column are divided into the following descending regions, from the neck to the buttocks:
- Cervical – 7 vertebrae designated as C1-C7
- Thoracic – 12 vertebrae designated as T1-T12
- Lumbar – 5 vertebrae designated as L1-L5
- Sacrum – 5 vertebrae
- Coccyx – 4 vertebrae
InjuryMap, CC BY-SA 4.0, via Wikimedia Commons
CS occurs when the cartilage between the vertebrae in the neck wears down. It can also occur in the other regions of the spine, resulting in difficulty moving the head. As the body ages, poor posture leading to osteoarthritis (OA) is a primary cause of CS (3). This often is the result of a lifetime of sitting for long hours with the head thrust forward. This posture can result in nerve compression in the neck and affect the nerves leading down the rest of the spinal cord. This can result in neck pain and weakness in the legs when walking, contributing to “slip and fall” accidents.

Let’s Simplify That:
The spine consists of a series of small bones, called vertebrae, cushioned by cartilage to prevent friction. CS occurs when the cartilage in the neck deteriorates, leading to pain and restricted movement. Factors such as prolonged poor posture can exacerbate this condition, resulting in neck discomfort and mobility issues that could increase the likelihood of falls.
Diagnosis and Management of Cervical Spondylosis
Diagnosis of CS is typically made following a thorough medical exam. However, tests such as x-ray, MRI, and/or a nerve conduction study may be performed. The treatment for CS depends upon its cause as well as its severity level. The following are the usual options for the treatment of non-severe CS (4):
- A course of physical and/or occupational therapy (PT and/or OT)
- Placing ice or heat to the neck to relieve neck pain for a maximum of 15 minutes several times per day (as recommended by a healthcare provider)
- Wearing a soft neck collar or brace
- Over-the-counter pain relievers
If CS is diagnosed as severe, steroid injection in the neck, radiofrequency ablation (heat applied to a nerve to dull pain transmission), or surgery may be recommended (5).
Putting It Plainly:
Medical professionals diagnose CS through physical examinations and tests like X-rays. Treatments vary from non-invasive methods such as physical therapy and applying heat or ice, to medication for pain relief. In severe cases, more intensive treatments like steroid injections or surgery may be necessary.
Understanding Heart Palpitations
Heart palpitations can have diverse causes and lead to a heart disorder if they occur too frequently over a lengthy period of time. The following list outlines the commonly-described symptoms of heart palpitations (6):
- Heart beating too fast
- Heartbeat fluttering rapidly
- Heart “flip-flopping”
- Heart pounding
- Heart skipping beats
Causes of Heart Palpitations:
Among the most frequent causes of heart palpitations at any age are emotional stress and anxiety. These factors trigger the increased release of two hormones in our bodies, adrenaline and cortisol, which in turn causes an increase in heart rate and blood pressure. Eventually, frequent heart palpitations can lead to a heart disorder called arrhythmia. This heart disorder is characterized by permanent, irregular contractions of the heart muscle.
Let’s Simplify That
Heart palpitations are characterized by sensations of a racing, fluttering, or irregular heartbeat. They can be induced by stress and anxiety, which elevate adrenaline and cortisol levels, accelerating heart rate. Persistent palpitations may lead to arrhythmia, a condition where the heart beats irregularly permanently.
Atrial Fibrillation (AF) and Stroke Risk:
A common cause of heart palpitation is Atrial Fibrillation (AF). AF is the most common type of arrhythmia and is identified by a sudden, rapid heartbeat (7). AF is a disorder of the normal beating of the heart’s upper chambers (two atria). That irregular beating causes a temporarily-reduced blood flow to the lower heart chambers (two ventricles). For this reason, AF can cause heart failure. The chance of having AF increases with age, and people living with AF are at five-fold increased risk of having a stroke (8).
Six other causes of sudden palpitations are (9):
- Excessive exercise that strains the heart muscle Exercise routines that are particularly intensive, such as HIIT (High Intensity Interval Training) and rowing
- A congenital heart muscle abnormality
- A hormonally-linked disorder such as Addison’s disease or hyperthyroidism
- Stimulants such as nicotine, coffee, amphetamines, cocaine, and some prescription medications
- High fever and/or extreme fatigue
- Hormonal changes caused by menstruation, pregnancy, or menopause
Occasional palpitations are not damaging to the heart, but chronic palpitations often result in an arrhythmia. Given that palpitations can be a symptom of a more serious heart disorder, individuals experiencing palpitations should undergo a medical examination to assess their heart function.
Breaking it Down:
AF, a common arrhythmia, significantly increases the risk of heart failure and stroke. It is characterized by rapid heartbeats that disrupt normal blood flow. Factors such as excessive exercise, certain medical conditions, stimulant use, and hormonal fluctuations can also provoke palpitations. When these palpitations are chronic, they can lead to an arrhythmia and therefore, AF.
Why Stimulants Cause Palpitations:
As they enter the bloodstream, stimulants cause blood pressure to temporarily spike. This is true of any stimulant regardless of whether the drug is legal or illegal. The resulting spike in blood pressure reduces blood flow through the arteries, so the heart has to pump harder for arterial blood to reach the heart. Following stimulant intake, palpitations are often experienced as a consequence of the sudden spike in blood pressure and increased heartbeat.
A prolonged use of stimulants can cause a heart arrhythmia to develop. In a Harvard Health article in 2022, the author noted that hospital admission for a heart disorder among prescription stimulant users (within their first 30 days of use) was 40% higher than their counterparts who were non-users of prescription stimulant medications (10). Strong evidence has existed for decades that smoking nicotine-containing products or the use of nicotine in other forms increases the risk for AF, as well as other cardiovascular disorders (11).
The Simple Explanation:
Stimulants raise blood pressure abruptly, forcing the heart to pump more vigorously. Chronic use can cause arrhythmia. Nicotine use, in particular, is linked to heightened cardiovascular risks.
Diagnosis and Management of Heart Palpitations and Heart Arrhythmias
As discussed above, palpitations have many causes. Therefore, diagnosing that cause will be a medical provider’s initial focus. The following are some of the usual diagnostic tests ordered after a physical exam (12):
- Electrocardiogram (EKG)
- Wearing a heart Holter monitor for a 24 hour period or longer
- Echocardiogram (also termed a cardiac ultrasound)
Treatment for an arrhythmia depends upon its type and whether it results in an abnormally slow, fast, or irregular heartbeat. For AF, the three usual treatment options are (13):
- Medications
- Cardioversion therapy (electrical shocks to reset the heart’s rhythm)
- Surgery
If mental or emotional stress is causing the palpitations, beginning a meditation practice or utilizing another relaxation technique such as biofeedback may be recommended to by a healthcare provider. Maintaining control over one’s anxiety levels is crucial to prevent the excessive release of the cortisol hormone, which can elevate the risk of heart disease.
Simplified Summary:
Identifying the underlying cause of palpitations is crucial. Diagnostic tests, including EKGs and heart monitoring, guide treatment strategies. These may involve medications, cardioversion therapy, or surgery. Stress management techniques are also recommended to mitigate heart disease risks.
The Connection between Cervical Spondylosis, Heart Palpitations, and Arrhythmia
Daily episodes of pain due to Cervical Spondylosis (CS) can increase a person’s anxiety level. As discussed above, emotional stress and anxiety can trigger heart palpitations through increased release of adrenaline and cortisol. Living with these conditions can interfere with activities someone enjoys and decrease their overall quality of life. This can lead to depression, exacerbating feelings of pain and causing a cyclical worsening of physical and mental health (14). If left unchecked, stress from pain can lead to heart arrhythmia and increased risk of stroke. Thus, coping with CS and/or heart palpitations requires not only healthcare interventions but also mental health therapy. By employing various strategies, individuals can break the downward spiral of pain and anxiety.
Recent research suggests another potential connection between CS and heart palpitations through the Sympathetic Nervous System (SNS), which controls involuntary body functions such as heartbeat. According to a study conducted in 2018, it is proposed that impairment of the CS nerve affecting the SNS may result in the occurrence of heart palpitations and arrhythmias (15). There have not yet been enough similar research studies to determine if such a connection actually exists.
In Simpler Terms:
Neck pain from CS can cause stress, which can lead to heart palpitations and even more serious heart issues. It’s important to take care of both physical pain and mental health to break this cycle. Plus, scientists are studying how neck pain might directly cause heart problems through the nervous system, but they’re still working on understanding how it all fits together.
Cervical Spondylosis, Heart Palpitations, and Stroke Risk
CS and heart arrhythmias can both increase the likelihood of a blood clot forming and traveling to the brain. As a major cause of stroke, these blood clots signify the link between heart palpitations and CS to the onset of stroke.
Many medical research studies over the past 50 years have shown that, as we age, the risk of acquiring both CS and arrhythmia increases. The lack of regular exercise can result in cervical spondylosis and a heart arrhythmia after age 60. Therefore, engaging in regular daily exercise through a person’s lifetime may prevent them developing both CS and heart arrhythmia, as well as decreasing their risk of stroke.
Since lifestyle factors such as smoking and obesity also increase the risk for stroke, making needed lifestyle changes to lose weight and quit smoking is very important. For individuals who have previously experienced a stroke, receiving continuous medical care is crucial to facilitate recovery and prevent the onset of secondary complications. This can include a referral for physical therapy, occupational therapy, and mental health counseling. Making needed lifestyle changes as a stroke survivor still matters and can lower the risk for another stroke.
In Easier Terms:
Chronic pain from CS can elevate stress levels, potentially leading to heart palpitations and arrhythmias, thereby increasing stroke risk. Preliminary research suggests a direct link between CS and heart rhythm issues via the nervous system, though further studies are needed to confirm this.
Conclusion
As people age, they face an elevated risk of developing cervical spondylosis (CS). The neck region becomes particularly susceptible to CS induced by osteoarthritis, exacerbated by the daily strain imposed on the neck and further intensified by persistent poor posture. Engaging in regular daily exercise is key to maintaining well-being later in life.
The pain and immobility often experienced with moderate-to-severe CS can trigger chronic anxiety and stress-induced heart palpitations. Other causes of heart palpitations include the overuse of stimulants and excessive physical exertion that strains the heart.
However, chronic anxiety is the primary cause and can lead to the development of an arrhythmia heart disorder, the most common of which is Atrial Fibrillation (AF). The risk for developing an arrhythmia, and especially AF, increases with age. Living with AF increases the risk for stroke with the potential of a blot clot forming and traveling to the brain.
It is a good idea to consult with a medical provider to rule out CS or a heart disorder such as arrhythmia if one is experiencing neck pain or palpitations. By obtaining early treatment and management for whatever health disorders are diagnosed, one can avoid having these lead to more disabling and potentially life-threatening conditions. By employing this strategy, In this way, a person can better preserve their overall quality of life as they age.
References:
- OrthoInfo. [American Academy of Orthopaedic Surgeons (AAOS)]. Cervical Spondylosis (Arthritis of the Neck). Webpage: https://orthoinfo.aaos.org/en/diseases–conditions/cervical-spondylosis-arthritis-of-the-neck
- DeSai C, Reddy V, and Agarwal A. (Updated 2023). Anatomy, Back, Vertebral Column. In: StatPearls [Internet]. StatPearls Publishing: Treasure Island, FL. Webpage: https://www.ncbi.nlm.nih.gov/books/NBK525969/#:~:text=The%20vertebral%20column%20(spine)%20defines,up%20the%20axial%20skeletal%20system.
- Ferrara LA. (2012). The biomechanics of cervical spondylosis. Advances in Orthopedics 2012: 493605. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3287027/
- Cleveland Clinic [Cleveland, OH]. Cervical Spondylosis. Webpage: https://my.clevelandclinic.org/health/diseases/17685-cervical-spondylosis
- Cleveland Clinic [Cleveland, OH]. Cervical Spondylosis. Webpage: https://my.clevelandclinic.org/health/diseases/17685-cervical-spondylosis
- Mayo Clinic. Heart palpitations. Webpage: https://www.mayoclinic.org/diseases-conditions/heart-palpitations/symptoms-causes/syc-20373196
- Centers for Disease Control (CDC). Atrial Fibrillation Webpage: https://www.cdc.gov/heartdisease/atrial_fibrillation.htm
- Medical University of South Carolina (MUSC). Stroke: Stalker of Our Aging Population. Webpage: https://muschealth.org/medical-services/geriatrics-and-aging/healthy-aging/stroke#:~:text=About%2075%20percent%20of%20strokes,double%20every%20decade%20after%2055.
- American Heart Association (AHA). What is Atrial Fibrillation? Webpage: https://www.heart.org/en/health-topics/atrial-fibrillation/what-is-atrial-fibrillation-afib-or-af
- Harvard Health Publishing [Harvard Medical School]. (February 1, 2022). How stimulants may affect your heart. Webpage: https://www.health.harvard.edu/heart-health/how-stimulants-may-affect-your-heart
- Benowitz NL, and Burbank AD. (2016). Cardiovascular toxicity of nicotine: Implications for electronic cigarette use. Trends in Cardiovascular Medicine 26(6): 515-523. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4958544/
- Mayo Clinic. Heart palpitations. Webpage: https://www.mayoclinic.org/diseases-conditions/heart-palpitations/diagnosis-treatment/drc-20373201
- Mayo Clinic. Atrial fibrillation. Webpage: https://www.mayoclinic.org/diseases-conditions/atrial-fibrillation/diagnosis-treatment/drc-20350630
- Sheng J, Liu S, Wang Y, et al. (2017). The Link between Depression and Chronic Pain: Neural Mechanisms in the Brain. Neural Plasticity 2017: 9724371. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5494581/
- Lin SY, Hsu WH, Lin CC, et al. (2018). Association of Arrhythmia in Patients with Cervical Spondylosis: A Nationwide Population-Based Cohort Study. Journal of Clinical Medicine 7(9): 236. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6162845/
- Zathar Z, Karunatilleke A, Fawzy AM, et al. (2019). Atrial Fibrillation in Older People: Concepts and Controversies. Frontiers in Medicine 6: 2019. Webpage: https://www.frontiersin.org/articles/10.3389/fmed.2019.00175/full
- Johns Hopkins Medicine [Baltimore, MD]. Palpitations. Webpage: https://www.hopkinsmedicine.org/health/conditions-and-diseases/palpitations
- Parikh NS, Parasram M, White H, et al. (2022). Smoking Cessation in Stroke Survivors in the United States: A Nationwide Analysis. Stroke 53: 1285-1291. Webpage: https://www.ahajournals.org/doi/10.1161/STROKEAHA.121.036941
- Sharma S, Merghani A, and Mont L. (2015). Exercise and the heart: The good, the bad, and the ugly, European Heart Journal 6(23): 1445-1453. Webpage: https://academic.oup.com/eurheartj/article/36/23/1445/2293352
- Heart&StrokeTM [Heart and Stroke Foundation of Canada, Toronto, Canada]. Atrial fibrillation. Webpage: https://www.heartandstroke.ca/heart-disease/conditions/atrial-fibrillation#:~:text=Untreated%20atrial%20fibrillation%20puts%20you,the%20grooves%20of%20the%20heart.