A mini stroke is medically termed a Transient Ischemic Attack (TIA) and it is caused by a temporary blood flow blockage in the brain that causes brain cell damage or destruction. Differing from a stroke, a TIA presents symptoms that are typically short-lived.
Experiencing a mini stroke increases your risk of experiencing a full stroke. Symptoms of this serious health condition are often sudden onset weakness on one side of the body, difficulty speaking, and other symptoms suggesting stroke. However, unlike a full ischemic stroke, these symptoms rapidly dissipate. TIAs occur in at least 240,000 people in the US every year, and up to 20% of people who have a TIA experience a stroke within 90 days (1, 2).
The primary purpose of this article is to provide an understanding of the various causes of a mini stroke or TIA, its range of possible symptoms, how it is diagnosed and treated, and how to prevent it as well as the potential consequences of experiencing numerous mini-strokes over time.
Understanding Stroke
There are two main types of stroke: ischemic stroke and hemorrhagic stroke (3). In ischemic stroke, a clot in the bloodstream either travels to the brain or occurs within the brain. That clot creates a blockage of blood flow to the affected part of the brain, resulting in nerve cell impairment and/or brain cell damage or death. In a hemorrhagic stroke, bleeding in the brain itself causes the nerve cell and/or brain cell death. A burst brain aneurysm (in an artery or vein) is a cause of hemorrhagic stroke, but not the only cause. Notably, around 87% of all strokes are ischemic strokes (4).
Besides destruction of nerve and brain cells, strokes cause damage to the brain’s neural pathways that transmit “messages” to the spinal cord and other parts of the brain. Therefore, a stroke can impact motor skills, cognition, speaking and/or comprehending language, and other normal functional abilities depending upon the location of the brain damage.
In contrast to strokes that may take hours to develop and have symptoms that last days or years, Transient Ischemic Attacks (TIAs) typically last only 15 minutes or less and have symptoms that can last only 24 hours (5). Because TIAs are short-term in onset and symptom duration, some survivors of mini strokes do not even realize that a TIA has occurred because signs of a stroke were less detectable and also quickly went away.
Stroke vs. Mini Stroke
TIAs and stroke share many of the same causes. One of the foremost causes of a stroke is hardening of the arteries (or atherosclerosis), in which plaque builds up in the walls of arteries. Atherosclerosis is most often caused by a chronically-high cholesterol level in the blood. Pieces of plaque can break off and cause a blood clot, which can block blood flow (6). When blood flow to the brain is blocked, a stroke occurs. Atherosclerosis that occurs in the carotid arteries, which bring blood to the brain, are especially associated with stroke. This is also the case in TIAs. For other causes of stroke, read about the impact of stress, and our guide to understanding stroke.
For those who have experienced a stroke, the overall risk for recurrent stroke is 26% within five years of the first stroke (7). This is why understanding the causes, symptoms, and preventions is so critical.
The most common pre existing risk factors for TIA in adults are:
- Hypertension (high blood pressure)
- High blood cholesterol level
- Poorly controlled diabetes (all types)
- Carotid artery narrowing or plaque build-up
- Heart rhythm disorders (such as atrial fibrillation
- A past history of TIA or stroke
Causes that are less publicly recognized are those who are living with Sickle Cell Disease (SCD) are at an especially high risk of TIAs, along with those living with poorly controlled epilepsy (8, 9). Furthermore, TIAs are strongly associated with Traumatic Brain Injury (TBI), due to these events:
- Violent blow to the head
- Blast-induced brain trauma, such as often experienced by military members serving in areas of armed conflict
- Moderate-to-severe concussion resulting from any cause
As mentioned earlier, the crucial difference between a TIA and a stroke is that TIA symptoms are usually short lived. This means that the one-sided weakness, confusion, or inability to speak typically disappears quickly in the person experiencing a TIA, and within 24 hours at most (10). If more TIAs occur after the first one, the likelihood of a slower return to baseline is increased, and recurrent TIAs are more likely to result in symptoms that do not resolve.
Symptoms of Mini Stroke
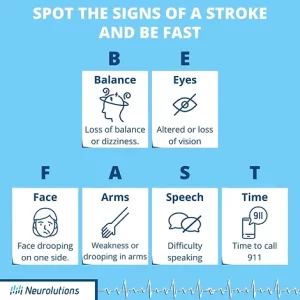
Symptoms of TIAs can include any or all of the following (11, 12):
- Sudden numbness or weakness in the face, upper extremity, or leg, and especially on one side of the body
- Sudden loss of coordination or loss of balance capacity
- Sudden mental confusion
- Sudden difficulty speaking or comprehending speech
- Sudden onset of seeing “double” or blindness
- Sudden severe headache with no known cause, and usually in the presence of other common TIA symptoms
Besides physical and cognitive symptoms (such as difficulty concentrating), both TIAs and strokes can result in increased depression and/or anxiety.
How is a Mini Stroke Diagnosed?
Mini strokes are most often diagnosed by physicians based on prior medical history in combination with a physical exam and lab test results. It can be far more difficult for clinicians to diagnose a mini stroke than a full-blown stroke, because the signs disappear. While CAT (Computed Tomography Scans) and MRI (Magnetic Resonance Imaging) scans are often used as tools to diagnose both stroke and TIA, the TIA may have passed by the time the patient receives the scans.Therefore, the scans may not demonstrate any observable abnormality. In contrast, CAT and MRI scans typically reveal brain injury or related abnormalities when there are larger and more persistent strokes.
Given that individuals who suspect they are experiencing strokes are typically advised to seek immediate medical care in a hospital, many people experiencing TIAs are first diagnosed in the emergency department. This is the reason CAT scans and/or MRIs are so often used by emergency medical providers in diagnosing a TIA, even though a conclusive diagnosis may not be apparent solely from the scans (13). On the other hand, CAT and/or MRI scans may be able to rule out another cause for the patient’s symptoms that can “mimic” a TIA, such as abnormally low blood sugar or a urinary tract infection.
In addition to diagnostic tests and labs, a comprehensive neurological examination will be performed to specify characteristics of symptoms, gauge severity of symptoms, and understand the impact the episode has on the individual’s function.
Treatment of Mini Stroke
If you or someone you know is experiencing symptoms that resemble a stroke as noted earlier, it is important to call 911 or get to the closest ED as soon as possible.
In the case of a high-risk TIA (especially if there is evidence of a clot in the brain), a medical provider may order tissue plasminogen activator (tPA) to serve as a clot-busting pharmaceutical treatment to reduce potential tissue damage caused by the blockage. The standard window of time intravenously (IV) it typically is administered is 4.5 hours following stroke symptom onset. There are risks associated with tPA administration, and therefore not everyone qualifies even if medical attention was received early.
Is Rehabilitation Needed after a TIA?
When a TIA is diagnosed, stroke-like symptoms are expected to have resolved. Most of the time, but not all the time, the individual returns to their prior level of function and does not have residual impairments.
However, it should be noted that there are individuals that were diagnosed with TIA yet still complain of physical, cognitive, emotional, and psychological changes. This could be due in part because the TIA episode and hospitalization led to stress, fatigue, and generalized weakness. A previously known medical condition may also get exacerbated, such as if the individual had vertigo spells, fibromyalgia, or was in the process of recovering from a knee replacement.
For this reason, it is important that the individual and their loved one closely monitor any lingering symptoms, overall health, and general functionality. If there is any concern that “things are not quite right,” it should be reported to the health care provider. If appropriate, occupational or physical therapy could be ordered to address balance, fall prevention, strength, cognitive impairment, and activities of daily living. Psychological intervention may also be needed if the individual is suffering from stress or anxiety caused by the episode.
Preventing Mini Stroke
Prevention of a stroke is a primary focus of TIA treatment. This can include treatment of a health disorder predisposing a person to TIAs. Both lifestyle changes and medication are often utilized as a strategy to prevent TIA. This may include blood-thinning medication to prevent stroke-causing blood clots from forming, surgery to treat narrowed carotid arteries, treatment with a daily statin medication to lower cholesterol, and an increased focus on better glucose control in poorly-controlled diabetes. Lifestyle changes including reducing obesity and smoking cessation (14).
People at ages 55 or older with other stroke risk factors such as hypertension are at increased risk for mini stroke (15). Adults who are obese and living with Type-2 diabetes are at significant risk of TIAs and stroke, so reversing obesity as soon as possible is a public health preventive strategy that will not only reduce the likelihood of progressing to Type-2 diabetes, but will also lessen the incidence of TIAs and strokes in the population as a whole. For TIA survivors, attending follow-up appointments with healthcare providers is an important strategy to prevent a second TIA.
For TIA survivors, a major barrier to reducing the risk of a second or third TIA (or a full-blown stroke) is the cognitive deficit that can result from the first TIA. Reduced attention/concentration, short-term memory loss, and reduced problem-solving ability are all potential cognitive impacts of a TIA. Those that have been diagnosed with a TIA (or are the loved one of a TIA survivor), keeping up with follow-up appointments with medical providers and engaging in specific lifestyle changes may be essential.
Are There Medical Disorders other than Stroke with Symptoms Similar to Mini Stroke?
There are numerous other disorders with symptoms similar to a TIA. Four of these disorders are:
- Seizure: These are sudden abnormal bursts of electrical activity in the brain, which can cause a variety of symptoms overlapping with those of a TIA. Seizures can be caused by a wide range of disorders including epilepsy, brain tumors (both benign and malignant), and stroke.
- Brain Tumors: Both benign and cancerous brain tumors can cause diverse symptoms similar to a TIA or stroke. Seizures, severe headaches, and double-vision are not uncommon in people with brain tumors, so such symptoms can be an indicator of a brain health disorder beyond that of a TIA.
- Migraines: Migraine headaches are typically characterized by a severe throbbing pain in the back of the head, and that is often accompanied by nausea, vomiting, and light-sensitivity. This can promote symptoms such as numbness in one side of the face and an inability to focus that can seem symptomatic of a TIA.
- Bell’s Palsy: This is a disorder that typically causes sudden weakness in one side of the face. Certain viruses have been linked to the onset of Bell’s Palsy, but not all causes are due to viruses; the exact cause in many afflicted people is unknown (16).
Ruling out other causes of the symptoms is imperative to correctly diagnose a person who appears to be experiencing a first TIA. It is also possible that a person can experience another brain health disorder in tandem with a TIA.
Conclusion – Summary of Key Points
The various causes of a stroke overlap with the causes of a Transient Ischemic Attack (TIA) or mini stroke, and having experienced a mini stroke increases a person’s risk for having a full-blown stroke. Both are injuries to the brain that can result in brain nerve damage and brain cell death.
Clots in the bloodstream or in the brain are the chief cause of both stroke and TIA, although brain bleeds are the second-most common cause. Unlike in stroke, the blood clots causing TIA are small enough or dissolve rapidly enough so that the blood flow blockage quickly releases. However, if the underlying cause of the TIA is not addressed, stroke risk is increased.
One of the primary differences between a stroke and a TIA is that the symptoms of a TIA typically appear for 15 minutes or less and for no more than 24 hours. Chronic high blood pressure, chronic high cholesterol, and poorly-controlled diabetes increase the risk of both TIA and stroke. Preventing and treating these conditions are vital strategies to reduce the chance that either will occur.
Similar to stroke, the location and severity of the brain injury is strongly linked to the type and severity of TIA symptoms experienced. Cognitive impairments such as poor concentration and short-term memory loss are often secondary consequences of a TIA. Therefore, people with a history of TIAs may need more support from family, friends, and/or caregivers to make lifestyle changes, remember to take their prescribed medication, and adhere to medical follow-up to prevent having a disabling stroke.
Following a diagnosis of TIA, it is critical to receive ongoing medical follow-up to find out the cause of the TIA, obtain treatment, and make the lifestyle changes required to prevent another TIA from occurring. Therefore, a stroke survivor may be able to ward off a catastrophic stroke that could result more permanent disability.
References:
- Rost, Natalia. (Last update: July 3, 2023). Patient education: Transient ischemic attack (Beyond the Basics). UptoDate.com [Wolters Kluwer] Webpage: https://www.uptodate.com/contents/transient-ischemic-attack-beyond-the-basics/print
- Cleveland Clinic. Transient Ischemic Attack (TIA). Webpage: https://my.clevelandclinic.org/health/diseases/14173-transient-ischemic-attack-tia-or-mini-stroke
- Centers for Disease Control (CDC). About Stroke. Webpage: https://www.cdc.gov/stroke/about.htm
- American Stroke Association. Ischemic Strokes (Clots). Webpage: https://www.stroke.org/en/about-stroke/types-of-stroke/ischemic-stroke-clots
- Hill MD, and Coutts SB. (2011). Preventing stroke after transient ischemic attack. Canadian Medical Association Journal 183(10): 1127-1128. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3134717/#:~:text=Transient%20ischemic%20attacks%20are%20sudden,last%2015%20minutes%20or%20less.
- Mount Sinai Health System, Cerebrovascular Center [New York, NY]. Atherosclerosis and Ischemic Stroke. Webpage: https://www.mountsinai.org/locations/cerebrovascular-center/conditions/stroke/atherosclerosis-ischemic-stroke#:~:text=Just%20as%20heart%20attacks%20are,called%20hardening%20of%20the%20arteries.
- Liu J, Zhu Y, Wu Y, et al. (2017). Association of carotid atherosclerosis and recurrent cerebral infarction in the Chinese population: A meta-analysis. Neuropsychiatric Disease and Treatment 13: 527-533. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5325114/
- Kirkham FJ, and Lagunju IA. (2021). Epidemiology of Stroke in Sickle Cell Disease. Journal of Clinical Medicine 10(18): 4232. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8469588/
- Epilepsy Action. (May 3, 2014: Last updated: September 28, 2022). Patients with Epilepsy Are at an Increased Risk of Subsequent Stroke: A Population-Based Cohort Study. Webpage: https://www.epilepsy.org.uk/patients-with-epilepsy-are-at-an-increased-risk-of-subsequent-stroke-a-population-based-cohort-study
- National Institute of Neurological Disorders and Stroke (NINDS). Transient Ischemic Attack (TIA). Webpage: https://www.ninds.nih.gov/health-information/disorders/transient-ischemic-attack-tia#:~:text=Most%20symptoms%20of%20a%20TIA,in%20one%20or%20both%20eyes
- Mayo Clinic. Transient Ischemic Attack (TIA). Webpage: https://www.mayoclinic.org/diseases-conditions/transient-ischemic-attack/symptoms-causes/syc-20355679
- American Stroke Association. Transient Ischemic Attack (TIA). Webpage: https://www.stroke.org/en/about-stroke/types-of-stroke/tia-transient-ischemic-attack
- Baghshomali S, Bishop L, Hiestand B, et al. (2015). Is CT Scan in Patients with Suspected TIA Necessary: A quality improvement initiative (P2.307). 84(14 Supplement): P2.307. Neurology Webpage: https://n.neurology.org/content/84/14_Supplement/P2.307
- Coutts SB. (2017). Diagnosis and Management of Transient Ischemic Attack. Continuum (Minneapolis Minn) 2017 23(1): 82-92. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5898963/
- Khare S. (2016). Risk factors of transient ischemic attack: An overview. Journal of Midlife Health 7(1):2-7. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4832890/
- Mayo Clinic. Bell’s palsy. Website: https://www.mayoclinic.org/diseases-conditions/bells-palsy/symptoms-causes/syc-20370028