For all of us, normal posture is an automatic movement that develops a child and involves trunk control, head control, mobility, the ability to tell where your body is in space, and the ability to bear weight or shift weight in all directions without falling over. Normal postural control allows for automatic and continual adjustment to all movements with all activities and allows one to regulate one’s body.
When neurological damage occurs, normal postural control and tone (normal tension in the muscles which help us move correctly) can be disrupted. Abnormal tone can lead to significant impairments in reflexes, balance, and control of all voluntary motor movements. Upon central nervous system dysfunction, decorticate or decerebrate posturing can take place based on the location of the injury.
What’s the Difference Between Decorticate and Decerebrate Posturing?
Decorticate Rigidity
Decorticate posturing results from damage to the cerebral hemispheres. In turn, this causes interruption to the corticospinal tracts which emerge from the cortex and send voluntary motor messages to all extremities. Decorticate rigidity presents with arms bending and wrists and hands clenched in flexion (bent inward like squeezing tightly).
Decerebrate Rigidity
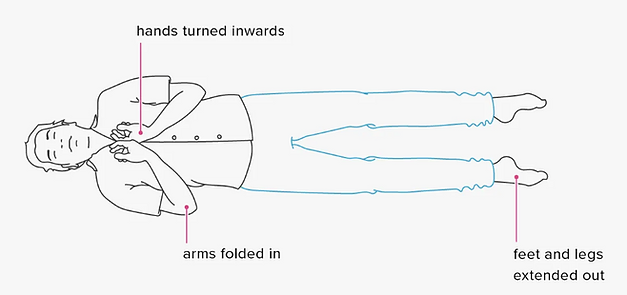
Decerebrate posturing occurs when damage to the brainstem and the extrapyramidal tracts is present, interfering with the process of sending involuntary motor messages from the brainstem to all limbs. For reference, the brainstem is a structure that connects the brain to the spinal cord and regulates many automatic functions of the body. Although more common than decorticate rigidity, decerebrate is associated with a poorer prognosis and survival rate.

Decerebrate positioning includes:
- arms and legs held straight out into extension (i.e. straight; not bent)
- the toes pointed downward in extension
- the head and neck arched and extended backward
- Postural deficits: Postural deficits develop as a result of an imbalance in muscle tone throughout the body. This can be caused by decorticate or decerebrate rigidity but can also occur over time by the implementation of ineffective strategies to compensate for impaired motor control. This includes delayed or absent righting reactions or other deficits in motor control caused by impairments in vision, cognition, or proprioception.
- Righting Reactions: Righting reactions refer to the ability to keep the head in an upright position. Without effective righting reactions, the individual will have difficulty with mobility and everyday activities such as getting out of bed.
Are you finding this article helpful? If you or a loved one has been impacted by stroke, the IpsiHand could help. Learn more about IpsiHand.
What Causes Decorticate and Decerebrate Posturing?
Decorticate and decerebrate rigidity and posturing are the results of neurological damage usually due to traumatic brain injury or a non-traumatic brain injury such as a stroke. Specifically, upon decerebrate rigidity, caused when a lesion in the midbrain, pons, or diencephalon. Decorticate rigidity occurs when lesions occur in the cortical white matter, internal capsule, thalamus, cerebral peduncle, and basal ganglia.
How Can You Treat Decorticate or Decerete Posture?
A physical therapist or occupational therapist will address decorticate to celebrate treatment for postures, and various treatments for postural impairments beginning with an evaluation of impairments related to positioning, posturing, and rigidity. Posturing deficits can be treated with interventions:
- Positioning: External equipment can be used to support and promote correct posture and prevent deformities. Using specialized wheelchairs with lateral supports, hardbacks, leg support, and arm troughs can allow for ability within the positioning. Functional seating positioning such as reclining and tilting in space can also support placing the pelvis in a neutral position to allow the trunk, head, and neck to remain in the midline. A formal wheelchair and seating evaluation can help customize what is needed to promote correct posture within the stroke survivor’s needs and limitations. The use of splints of orthotics on the hand and feet can also promote appropriate joint positioning from the onset of decorticate or declebrate positioning in the hospital or at home.
- Mobility: Mobility does not refer just to walking. It can include things like bed mobility (i.e. turning the bed and sitting up to get to the edge of the bed) and bearing weight while sitting and standing. Physical therapy will address these needs as early as the ICU in some facilities and through all continuums of care. Occupational therapy is also addressing functional mobility within functional transfers and activities of daily living.
- Visual feedback: Visual feedback can be integral in assisting the individual to gain awareness and understanding of their environment and posture as well as how to correct it. A fair amount of individuals who are experiencing postural deficits are unaware they are leaning or pushing to one side of the body away from the midline. Placing a mirror in front of them or showing them videos/pictures of their positioning can be very helpful to build awareness.
- Tactile of verbal cues: Due to decreased awareness of midline and upright posture, stroke survivors can benefit greatly from a verbal reminder or light touch to the side at which they are leaning to correct back into the midline.
- Dynamic reaching activities and weight shifting: Once the stroke survivor has gained increased awareness of the midline and their body in space, integrating reaching activities to left, right, and across the midline can be very beneficial to begin working on weight sifting and correction of balance. This can only be initiated if safe to do so from a supported sitting or standing position.
- Self-care and instrumental activities of daily living: Beginning to address daily living skills such as bathing and dressing, brushing teeth, and eating is vital to promote increased awareness and posture in everyday life. Although posture and tone can greatly interfere with performance, it is necessary to try activities of daily living when safe with an appropriate set-up of environment.
- Medical Management: Medication management such as Botox or Baclofen or surgical intervention may be used to help increase comfort or for pain control. Speak with your physician about medication management of decorticate and decerebrate posturing.
Decorticate and decerebrate posturing can be very limiting in recovery following a stroke or a traumatic brain injury. It is important to seek proper guidance and treatment from a trained occupational and physical therapist. This is not an exhaustive list of treatment options for decorticate, decerebrate, and postural control deficits. Please speak with your healthcare team for continued education and guidance as this topic is extensive and imperative to address during recovery if any posturing impairment has occurred following a stroke.
References:
Pendleton and Schulta-Krohn (2006) Pedretti’s Occupational Therapy Practice For Physical Dysfunction: 6th Edition. New York, Elisver.




