Introduction to Pontine Strokes
If you or a loved one have had a pontine stroke or if you are a healthcare professional that is working with an individual who has had a stroke in this area of the brain, this overview will guide you in what you need to know to optimize your recovery.
To understand pontine stroke causes, symptoms, and strategies for recovery, it is first important to grasp the anatomy and functions of the structures that are involved with this specific type of stroke.
What is a Pontine Stroke?
A stroke, or a brain attack, results from a disruption of blood flow to the brain from a ruptured or blocked blood vessel.
A pontine stroke is a highly localized type that occurs within the brainstem. For reference, the brainstem is a structure that connects the brain to the spinal cord and regulates many automatic functions of the body, including blood pressure, breathing, swallowing, heart rhythms, facial sensations, and balance.
The pons, the middle and largest portion of the brainstem, is the specific structure that is damaged during a pontine stroke. The pons serves as a line of communication between the largest part of the brain (the cerebral cortex) and the portion of the brain on the back of the head (the cerebellum). Additionally, there are four cranial nerves (CN 5-8) that originate from the pons.
The pons plays a critical role in coordinating balance, facial sensations and movements, hearing, and equilibrium. It contributes to automatic functions, such as the sleep-wake cycle and regulation of breathing.

What causes a Pontine Stroke?
The pons receives blood supply from the basilar artery and two additional cerebellar arteries. Obstruction of blood supply caused by a clot or blockage (i.e. ischemia) to these arteries can cause a pontine stroke. When a hemorrhage is involved, it means the contributing arteries to the pons have ruptured or burst.
Pontine strokes are not extremely common when compared to other locations of strokes in the brain or brainstem.
Pontine strokes compromise about 7% of all ischemic strokes in which there is an obstruction of blood supply to the pons. (1) Pontine hemorrhages account for 10% of hemorrhages, with mortality ranging from 30-60%. (2)
Pontine strokes do not tend to be as massive as other strokes. However, they can be devastating when they happen because of all the vital structures that reside in the real estate of the pons. Damage to the corticospinal tract may occur, and this important pathway carries the information needed for movement between the brain and spinal cord.
Additionally, one or more of the four cranial nerves can be damaged and cause a variety of clinical symptoms. Finally, the pons itself plays a critical role in functions of the brainstem, and when there is damage, bodily functions such as respiration and circadian rhythms, often suffer.
What are the Risk Factors for Pontine Stroke?
Stroke research suggests that more than 90% of strokes are associated with 10 potentially modifiable risk factors (3).
Two of these established risk factors- longstanding high blood pressure and diabetes- are also leading risk factors for pontine stroke (4-6).
Research suggests that once you have had one stroke, you will be in a higher risk category for having another. Statistics show that 1 in 4 stroke survivors will have another yet another stroke (7).
Lifestyle modification can make a significant impact on the reduction of blood pressure and the management of diabetes to reduce the risk of stroke recurrence. Prevention of stroke is key, it is accomplished by a combination of a healthy diet, physical fitness, tobacco cessation, managing blood glucose, and controlling cholesterol (7).
It is important to note that in most cases, a second stroke will be more severe than the first stroke. It is very valuable to take incremental steps to make lifestyle changes that influence modifiable risk factors for stroke. Talk to your doctor, life coach, nutritionist, or therapist on how to accomplish these steps using a care plan that could save your life and future.
How to Spot the Warning Signs of a Pons Stroke Early On?
First, always be aware of these signs of a stroke of any type. Strokes of all types are considered an emergency, and immediate medical attention is needed to improve prognosis and receive critical care.
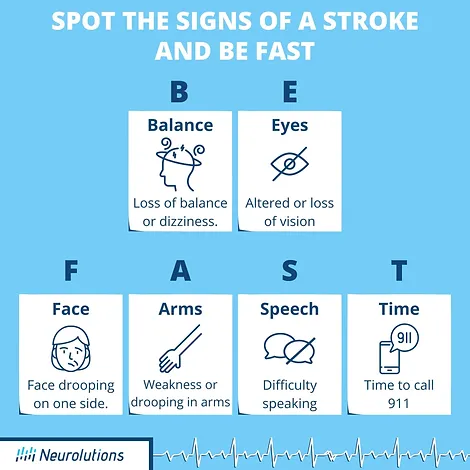
Use the acronym B.E. F.A.S.T. for guidance (7):
If a pontine stroke is occurring, there is a risk for respiratory compromise due to the pons’ role in breathing and blood pressure. This is an emergency as ventilation and intubation may be warranted. (8)
The individual may additionally present with sudden confusion, difficulty walking, poor equilibrium and balance, and difficulty speaking or understanding speech. Ataxia, or trouble coordinating movement, may be present in the leg on the same side that the stroke occurred. In tandem, there may be weakness on the opposite side of the body where the stroke occurred. Loss of facial sensation and weakness may occur on the same side that the stroke occurred in the pons.
What are the Clinical Signs & Symptoms of a Pontine Stroke?
Clinical presentation of a pontine stroke will vary depending on the area of the pons that was damaged. The following is a general description of several of the symptoms that could occur as a result of a pontine stroke. These symptoms may not only be present at the onset of stroke, but some may last into a chronic problem with different levels of severity.
- Coordination problems with arm or leg (ataxia on one side of the body)
- Weakness on one side of the body (hemiparesis)
- Impaired dexterity and weakness of the hand
- Slurred speech and/or trouble with speech pronunciation (dysarthria)
- Facial weakness and facial sensory disturbances
- Sensory deficits
- Difficulty with eye movements
- Difficulty swallowing (dysphagia)
- Vertigo and difficulty with equilibrium/balance
- Locked-in syndrome: a condition in which awareness and cognition is preserved, yet the individual has complete paralysis of voluntary muscles of the body aside from control of eyelids and eye movement.
What is the Prognosis for Pontine Stroke?
Prognosis can often be attributed to the location in the pons in which the stroke occurred. For example, unilateral and rostral to mid-pons strokes overall have more favorable prognoses and outcomes (9-11). . On the contrary, the poorer prognosis is correlated with bilateral and caudal pontine strokes. (12, 13)
When the pons is damaged, it is believed one of the consequences is an interruption of information exchange. This information conduction problem explains pontine stroke signs and symptoms, and it also asks the question, “What therapies are there to potentially ‘get around the block’ and/or generate brain signals that are compatible with secondary routes?”
What is the Treatment for Pons Syndrome?
The following is a list of common pons syndrome treatment that is utilized in medicine and rehabilitation to recover function and independence:
Address equilibrium and eye movement:
Eye stability, gaze, and tracking of ocular movements provide information to systems in the body that provides equilibrium and balance. This is commonly impacted during a pontine stroke. Therefore, it is highly important to retrain these systems and work on activities that partner with eye movement and balance. Occupational and physical therapists that specialize in “vestibular rehabilitation” in neurological conditions will be able to provide specific exercises to help progress with their tolerance to movement and skills of functional mobility.
Address facial weakness:
The basic idea behind initiating exercises for the facial muscles is to retrain the brain-to-nerve-to-muscle pathways. Although occupational and physical therapists may be trained in this area, speech therapists are often utilized in rehabilitation to address facial weakness and also sensation issues. Impairments in the face, mouth, or tongue can affect speech and swallowing.
Facial expression is commonly impacted by pons strokes, so beginning in front of a mirror, work on smiling, frowning, puckering the mouth, and blowing up the cheeks. Use the mirror to check the symmetry of the face and strive to be as “expressive” as possible.
There has been success with the utilization of NMES (a type of electrical stimulation) on the face to help with facial paralysis. (14) Talk to your physician and therapist to see if this is a treatment approach that is right for you.
Address coordination of the ataxic leg:
As stated earlier, it is a common presentation to have the leg on the same side that the pons stroke occurred, be clumsy, uncoordinated, and have difficulty with control (i.e. ataxia). This can lend to obvious problems with mobility and walking and can also be a safety concern due to a higher risk of falls.
Re-education of the affected limb might involve repetition of activities that work graded progression to a master of stance and swing of the leg. An example of this is forwards and backward stepping on targets on the floor to work on the calibration of movement and improve stepping accuracy. Physical therapy can help tailor exercises that address ataxia of the leg, while occupational therapists can help work on activities that promote the return of function and engagement in occupation as the legs gain coordination and control.
Address walking and mobility:
Walking can be very difficult for those who have suffered a pontine stroke. This is not just because of weakness and ataxia, but also because of the difficulties with their equilibrium and balance. Once the individual has worked on building stronger eye muscles needed for holding focus and also for tracking, walking should gradually be incorporated as part of the intervention.
Walking near walls or a structured area in which there are vertical boundaries not only helps with safety but might provide some visual and occasionally tactile feedback for the body. Physical therapists are equipped to address gait and mobility training so walking speed, coordination, endurance, and distance can improve.
Address weakness and fine motor control of the arm and hand:
Use a combination of resistance training (e.g. bands, tubes, weights, machines) and functioning strengthening using everyday objects around the home and community. So long that safety is not compromised, seek out as many opportunities as possible during daily tasks to open jars, hold onto cups, reach for items, and manipulate small objects.
Modifications and adaptations can be done as needed. Occupational therapists often play a role in restoring arm and hand function by working on arm weakness and fine motor impairments.
Address gradual increase of activity tolerance:
In the likelihood that regulatory functions like respiration and blood pressure were affected by the stroke in the pons, an individual may struggle with endurance during tasks and have limited tolerance for sustaining activities without having a strain on their cardiovascular system. Daily activities as well as rehabilitation efforts by both physical and occupational therapy usually require rest periods, a gradual increase in time spent engaging in tasks, and adherence to monitoring vitals.
Whether you are a health care professional or individual/ care provider that suffered a pontine stroke, it is important to always monitor vitals, especially blood pressure. This is important to have information on how the body is managing increased stress and stimulation, but also to be vigilant in the event that another stroke is around the corner.
Promote neuroplasticity using medical or rehabilitation treatments that show efficacy:
- Engage in activities that are high repetition, train specific to the task, and are motivating and meaningful.
- Talk to your neurologist or physician to learn about medications that are right for you or your loved one that may promote neuroplasticity in the motor system.
- There are also non-invasive therapeutic devices to try as a part of therapy. Brain-computer interface devices may help an individual generate cortical signals and provide secondary routes for relaying messages between the upper limb and the brain. (16)
Develop coping strategies while promoting the development of mental and emotional fortitude:
Cognition is generally not damaged by pontine stroke. This is excellent news because having good cognition is hugely important for getting the most out of therapy. Cognition is also crucial for having engagement and awareness to participate in interventions that promote restoration of function and returning to activities.
All members of the patient’s care team play a role in the empowerment of patients and care providers.
Pontine strokes, although small and local, have the potential to cause impairments in the automatic systems of our body, our sensory pathways, and voluntary movement systems. The prognosis for recovery varies from good to poor and may be dependent on the location within the pons. Rehabilitation can help maximize the potential for recovery, and should always be considered as a part of the recovery plan after a pontine stroke.
References
- Saia V, Pantoni L. Progressive stroke in pontine infarction. Acta Neurol Scand. 2009; 120:213–215.
- Wessels T, Möller-Hartmann W, Noth J, et al. CT findings and clinical features as markers for patient outcome in primary pontine hemorrhage. AJNR Am J Neuroradiol 2004; 25: 257–260
- O’Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, Rao-Melacini P, Zhang X, Pais P, Agapay S, Lopez-Jaramillo P, Damasceno A, Langhorne P, McQueen MJ, Rosengren A, Dehghan M, Hankey GJ, Dans AL, Elsayed A, Avezum A, Mondo C, Diener HC, Ryglewicz D, Czlonkowska A, Pogosova N, Weimar C, Iqbal R, Diaz R, Yusoff K, Yusufali A, Oguz A, Wang X, Penaherrera E, Lanas F, Ogah OS, Ogunniyi A, Iversen HK, Malaga G, Rumboldt Z, Oveisgharan S, Al Hussain F, Magazi D, Nilanont Y, Ferguson J, Pare G, Yusuf S; INTERSTROKE investigators. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016 Aug 20;388(10046):761-75. doi: 10.1016/S0140-6736(16)30506-2. Epub 2016 Jul 16. PMID: 27431356.
- Kumral E, Bayülkem G, Evyapan D. Clinical spectrum of pontine infarction. Clinical-MRI correlations. J Neurol. 2002 Dec;249(12):1659-70.
- Bassetti C, Bogousslavsky J, Barth A, Regli F. Isolated infarcts of the pons. Neurology. 1996 Jan;46(1):165-75.
- Gökçal E, Niftaliyev E, Baran G, Deniz Ç, Asil T. Progressive deficit in isolated pontine infarction: the association with etiological subtype, lesion topography and outcome. Acta Neurol Belg. 2017 Sep;117(3):649-654.
- Stroke.org
- (Malla G, Jillella DV. Pontine Infarction. [Updated 2022 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554418/).
- [PubMed PMID: 12529787]
- [PubMed PMID: 9099201]
- [PubMed PMID: 16324092]
- [PubMed PMID: 12529787]
- [PubMed PMID: 22343639]
- Choi JB. Effect of neuromuscular electrical stimulation on facial muscle strength and oral function in stroke patients with facial palsy. J Phys Ther Sci. 2016 Sep;28(9):2541-2543. doi: 10.1589/jpts.28.2541. Epub 2016 Sep 29. PMID: 27799689; PMCID: PMC5080171.
- Alawieh AM, Au Yong N, Boulis NM. Contralateral C7 Nerve Transfer for Stroke Recovery: New Frontier for Peripheral Nerve Surgery. Journal of Clinical Medicine. 2021; 10(15):3344. https://doi.org/10.3390/jcm10153344




